medication in the perinatal period part 2 of 3
What are the considerations of PREGNANCY and BREASTFEEDING with medications?
The reason why medication may be looked at with hesitation during pregnancy for anxiety and depression is the potential risk to the unborn baby, which I can appreciate as a mother myself. However, not looking after your mental health can impact the baby if you are not sleeping or eating.
+ Some classes of medication are considered safer in pregnancy and breastfeeding, so these would be considered FIRST LINE than other options.
+ When you are prescribed medication it is important to speak to your doctor and there are pregnancy categories of medications to help alleviate any concerns.
+ Like all medication, your doctor will always try to use the LOWEST dose for the SHORTEST time possible, taking in the consideration of where you are at.
+ In terms of breastfeeding, it is important to tell your doctor that you are breastfeeding so that is part of their decision making process. Looking for signs in your baby of any changes upon starting medication may be helpful; a rash, runny stools for example. If you are finding that there are signs in your baby or changes, then chat with your doctor to decide the best course of action.
+ Speak up about specific concerns you have, ask for the CMI (consumer medicines information) and ask the questions so that you have your concerns answered rather than sitting on them and festering.
Although a separate topic, what are the implications of medications for HG (hyperemesis gravidarum whilst pregnant?
Whilst nausea and vomiting is quite common is pregnancy with 69% experiencing it, HG is a severe form of nausea and vomiting. This only affects 1.1% of women, however, it can be very taxing in an emotional, psychological, physical, and financial capacity for the woman and her family.
Whilst it is not perinatal mental health specific, those impacted absolutely can have their mental health affected due to how they are feeling.
HG is defined as a severe form of nausea and vomiting with;
-symptoms starting early in pregnancy, before 16 weeks (typically between the 4th-10th week, with most symptoms resolved between 16-20 weeks)
-inability to eat and/or drink normally
-it limits their daily activities
-may show signs of dehydration and/or electrolyte imbalances
Women will be screened with the EPDS questionnaire and severity assessed by a PUQUE score. Medications are available to help with the symptoms, where managing symptoms is KEY and the main aim to optimise feeling your best.
There are SEVERAL medications to choose from, with first line through to third line therapies available, where usually one medication is commenced and its efficacy assessed, then dosage increased first before changing it.
The risk of not treating the HG can far outweigh the complications of not treating it, so it is important to manage the symptoms.
Complications listed from the NSW Health Guidelines include;
- malnutrition and loss of muscle mass
- hyponatraemia and hypokalaemia (severe electrolyte implications)
- venous thromboembolism
- abnormal thyroid and liver function
- placental dysfunction – which may be associated with an increased risk of small for gestational age babies, preterm birth, preeclampsia and placental abruption
- dehydration and renal failure
- haemorrhoids
- dental enamel erosion
- adverse impact on mental health, family unit, ability to perform usual duties and paid work
Whilst it can feel risky to take medication for HG whilst pregnant, the risks of severe nausea and vomiting are very high, therefore its impact on one’s mental health and emotional well-being IS vital to not ignore.
Know that medication is available, and to discuss all of the options with your doctor. Looking at which supplements and multivitamins you are taking, meal size, acidity levels and what factors make your symptoms better or worse are all important!
What are possible SIDE EFFECTS of each class of medication?
Medication for ANXIETY, DEPRESSION and INSOMNIA each work in different pharmacological ways, so the side effects that they exert will be different.
As a general indication or idea, side effects may include but not limited to as there are so many classes of medicines;
ANXIETY MEDICATION
Drowsiness, dry mouth, light-headedness, disorientation, effects on vision
DEPRESSION MEDICATION
Nausea, diarrhea, insomnia, drowsiness, dry mouth, dizziness, headache, anxiety, sexual dysfunction, blurred vision, constipation, loss of libido.
INSOMNIA MEDICATION
Impaired alertness the next morning, drowsiness, sleepwalking, dry mouth, taste disturbance
It is important when beginning a NEW medication to find out;
+ WHAT the side effects are
+ HOW LONG they should last for
+ WHAT to do if they occur
- Speak to your pharmacist and ask for the CMI (consumer medicines information) to run through all the effects to watch for.
- Some side effects can be short lived and resolve after a few days as your body gets used to it, for e.g. drowsiness
- Some side effects can be reduced by having it with food for e.g. nausea
- Some side effects can be long lasting but not cause too much trouble in your day to day life for e.g. dryness of the mouth
- Some side effects it can be crucial to watch out for it, especially those close to you, for e.g. suicidal ideations
Therefore, it is important to know about them before and have managed expectations about what may happen.
What is the side effects are causing a problem?
If the side effects are long lasting, affecting your quality of life, are not getting better or you are not happy with how they make you feel, then chat with your pharmacist who may have strategies to help minimize them (postural hypotension, get up slowly). If they still do not help, then chat with your prescriber who may be able to direct you on what to do.
Clear communication is key ALWAYS. Speak with the receptionist and hopefully they can get back to about an appointment or some instruction from the doctor.
Never stop the medication on your own accord because of side effects. It can cause more side effects or withdrawal symptoms, and the medication may be bringing benefit to your biochemistry and disrupting it may cause it to take longer to stabilise again.
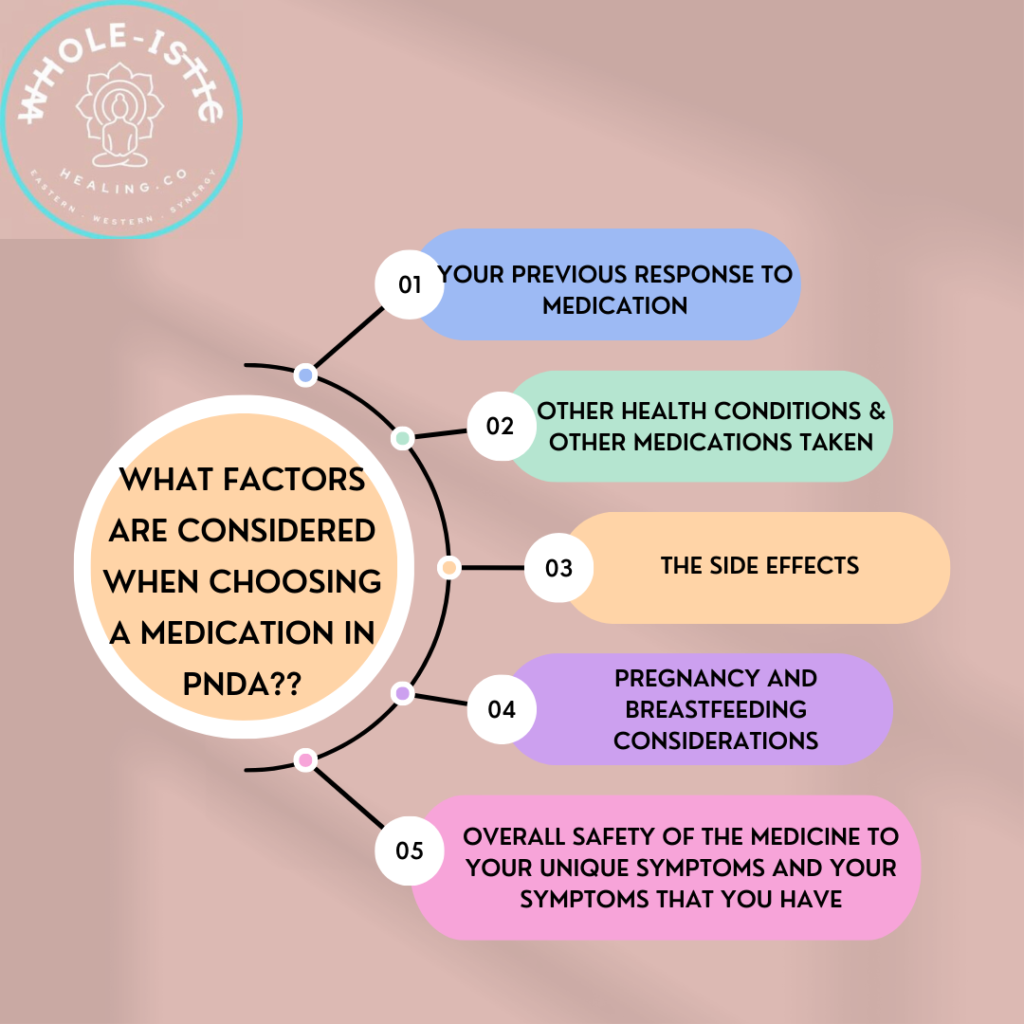
What are possible DRUG INTERACTIONS with medications for PNDA?
Each class of medications can interact with various other prescription medicines and over-the-counter medicines and supplements.
Therefore, it is VITAL to tell your doctor what other medicines you take so that they can decide which medication is the safest for you.
Therefore, it is VITAL to check with your pharmacist first before commencing any medicines OTC, even if you think they are safe. Various herbs can interact too, for example St John’s Wort can interact with the pill to reduce its efficacy and can impact how much antidepressant is in your system, so it is never advisable to combine OTC medicines without checking first.
As a general rule, ask every time; but know that certain PAIN, COLD/FLU MEDS, natural supplements can all have an impact so it can be dangerous! Below are some OTC considerations, as there are so many prescription interactions!
ANXIETY MEDICATIONS
Some cold and flu medicines, stimulants
INSOMNIA MEDICATIONS
Some cold and flu medicines, over-the-counter sleep medicines, some anti-histamines
DEPRESSION MEDICATIONS
St John’s Wort, some cold and flu medicines, some anti-histamines
What are the considerations with ALCOHOL whilst taking antidepressants/medications?
- Alcohol in itself acts as a depressant, it can affect mood and increase anxiety, so it can seem like you are not feeling any better but it may be the alcohol rather than the medicine not working.
- Alcohol can potentiate the drowsiness of medicines and can be dangerous with operating machinery and also cause respiratory depression, which can be fatal
- It places the liver under extra ‘strain’ or effort to metabolise various ‘foreign’ agents, so it would be safer not to have it to contend with
There are some medications you should not drink with at all, and others can be safer at least once a stable dose and condition have been established.
However, I would say that it is ALWAYS best to check with your pharmacist and doctor FIRST before combining alcohol with your medicines. It is not as straight forward as saying ‘no’ or yes, but to ask that question prior to combining it from your medicines expert!
What are some possible FOOD INTERACTIONS?
There is a class of medicines which can interact with various food types. It is unlikely that you would be prescribed it during pregnancy or breastfeeding, however, it is important to know if your medicine does interact with foods as it IS possible!
The class of medicines is called Monoamine Oxidase Inhibitors which can interact with foods containing tyramine. Whilst it is not common during the perinatal period, it may be worth asking the question just to be sure!
What happens if medications do not work for you?
If a medicine does not work, it can feel natural to just stop taking it. However, never do this!
Crystal clear communication is key here, always!
Chat with your doctor. Options they will decide based on your unique circumstance may be to;
+ increase the dose
+ add another medicine that works in a different way
+ slowly wean off that medicine and trial a different one
It will depend on you, your situation so there is no one size fits all.
However, NEVER just stop taking it as you can have severe side effects, withdrawal symptoms and put the body under a lot of strain. Medicines have different HALF lives, so knowing this is the foundation of understanding the changeover process so that it is SAFE.
Also the risk of not monitoring your mental health and symptoms is very important here. Tell your loved ones if you ever have been instructed to reduce or change medicines so they know what to watch for and look out for.
What happens when WEANING OFF medication (upon doctor’s advice & consultation only)
It depends upon which class of medicine you are taking and what dosage you are on! No one size fits all approach!
Some medicines can be reduced gradually and then stopped.
Others can be safely stopped.
Some need a washout period before starting a new medicine.
Some require a crossover regime where you commence a new one slowly whilst slowly reducing one.
The permutations and combinations are huge!
The important thing is to NEVER stop medicines on your own accord; only upon your doctor’s advice and CLEAR information as to HOW to do it.
Ask them what to watch out for, over what time period should you reduce, how long of a gap between starting a new medicine.
Then it is important to find out all the information you found out the first time;
+ how the new medicine works
+ potential side effects
+ interactions with alcohol, other medicines, food
+ how long it will take to work
+ how long to take it for
+ how and when to wean
Knowing this before you start is KEY! Health literacy is powerful and safer for you!