medication in the perinatal period
WHAT treatment is available for PND and PNDA?
- Psychotherapy (CBT, IPT, behaviour therapy, MBCT, counselling & more with a psychologist or counsellor or psychiatrist.
- Medications
- ECT (Electroconvulsive therapy)
Ideally, the first step is to see your GP or obstetrician who can refer you to the appropriate health care professional. It would be a ‘step up’ approach based on your UNIQUE circumstance and presenting symptoms.
In terms of medications, they usually are not used in isolation or alone; but ideally in combination with psychotherapy. In my case, my biochemistry WAS the underlying kink in my chain, & nothing would get through until my biochemistry was restored and I ‘sparked back to life’. The CBT thereafter was only a few sessions because it was a chemical reaction to hormones that derailed me and that was the CORE work that required correction.
However, I would always recommend the tandem use and gradual ‘step-up’ therapy and to trust in your health care team.
WHO should you see to obtain treatment?
I believe in seeing your GP or obstetrician FIRST. This is because they can;
- Prepare a mental health care plan and refer you to whom they believe is necessary (counsellor, psychologist, psychiatrist, mother baby unit (MBU))
- They can undertake DIFFERENTIAL DIAGNOSIS by ruling out other physical health conditions also through blood tests etc. for an underlying thyroid, endocrine, iron levels etc. This is VERY helpful to look after you ‘whole-istically’ and work out exactly what is happening
Then, once you see the referred professional, medication MAY be a piece that they consider as part of looking after your specific symptoms of the condition. However, it should ALWAYS be AUGMENTED with psychotherapy; and often, psychotherapy alone is sufficient!
WHAT medications exist for PND and PNDA and HOW do they work?
Each class of medication can treat SPECIFIC symptoms and they can ALL work in different ways. There can be prescription medications to treat;
- Insomnia (various classes of medications)
- Depression (various classes of medications; SSRI’s, SNRI’s, TCA, MAOI’s, selective MAOI’s, tetracyclic antidepressants; not that all of these are used on pregnancy/post-partum patients!)
- Anxiety (various classes of medications; antidepressants listed above, benzodiazepines)
- Specific symptoms in OCD, PTSD, psychosis, bipolar disorder (various classes of medications; above mentioned, lithium & antipsychotics)
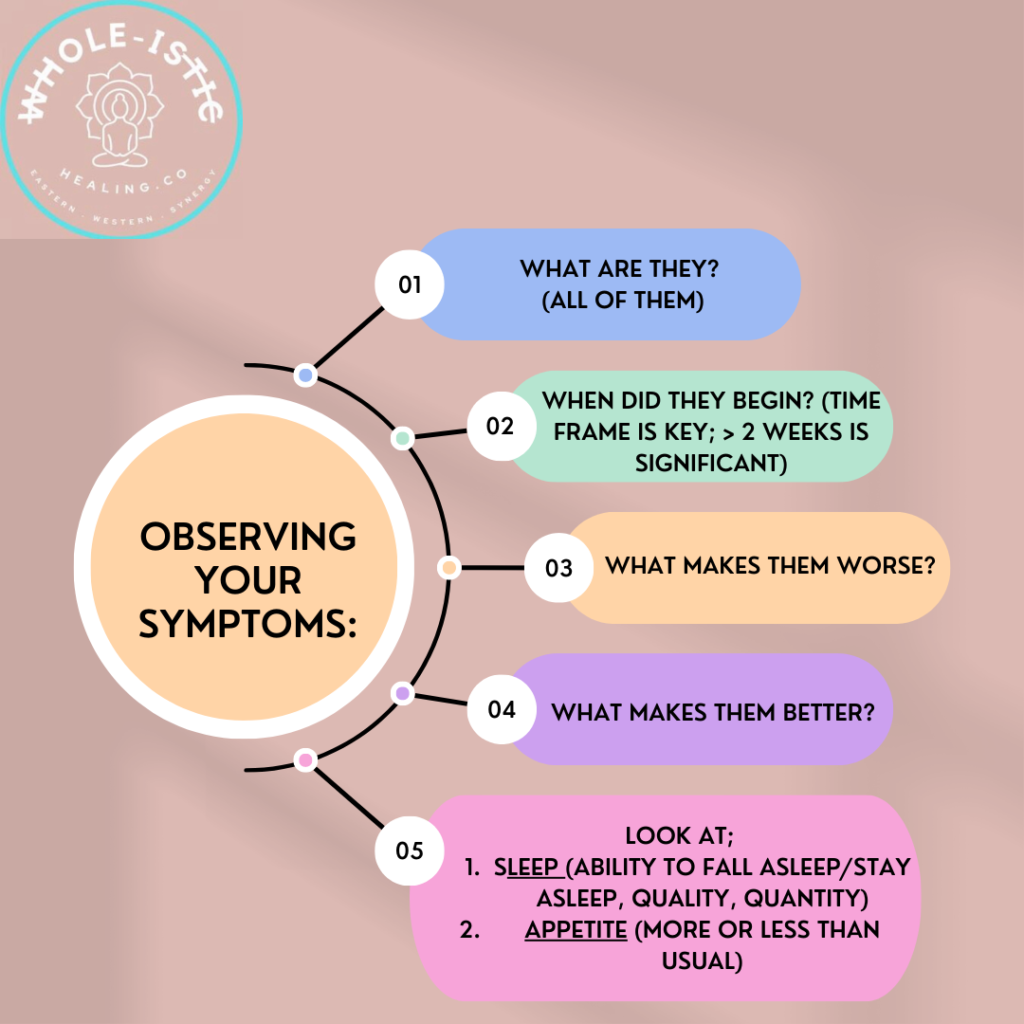
It is therefore very important to discuss with your doctor about your SPECIFIC SYMPTOMS, as well as;
- What are your symptoms? ALL of them!
- When did they begin? (Time frame is key; TWO or MORE weeks of continual symptoms is the gauge to determine the condition)
- What makes them worse?
- What makes them better?
- Looking at sleep (quality, ability to fall asleep, stay asleep, quantity; more or less than usual)
- Looking at appetite (more, less than usual)
- You can keep a journal and make note of your observations
- Ask a loved one what they notice (I was not able to tell you anything!)
- Ask a loved one to come with you to the appointment if that would help
Then, the doctor may prescribe ONE or TWO different CLASSES of medications. Without going into the pharmacology of them all, suffice to say that each CLASS of MEDICINE exerts a different affect (to serotonin, dopamine, noradrenaline, GABA and many more pathways!)
An SNRI, for example, is a serotonin and noradrenaline reuptake inhibitor, so inhibits the reuptake of those neurotransmitters! This reduced ‘clearance’, can reduce depression symptoms & reduce anxiety symptoms, which may alone reduce insomnia symptoms.
However, it is up to your prescribing physician to make their best judgement call on WHAT they feel is best for you based on your individual symptoms.
You may only require ONE medication, or you may require two initially and then wean off one when stable, or it could be trial and error to see WHAT is effective for you & tailor it accordingly.
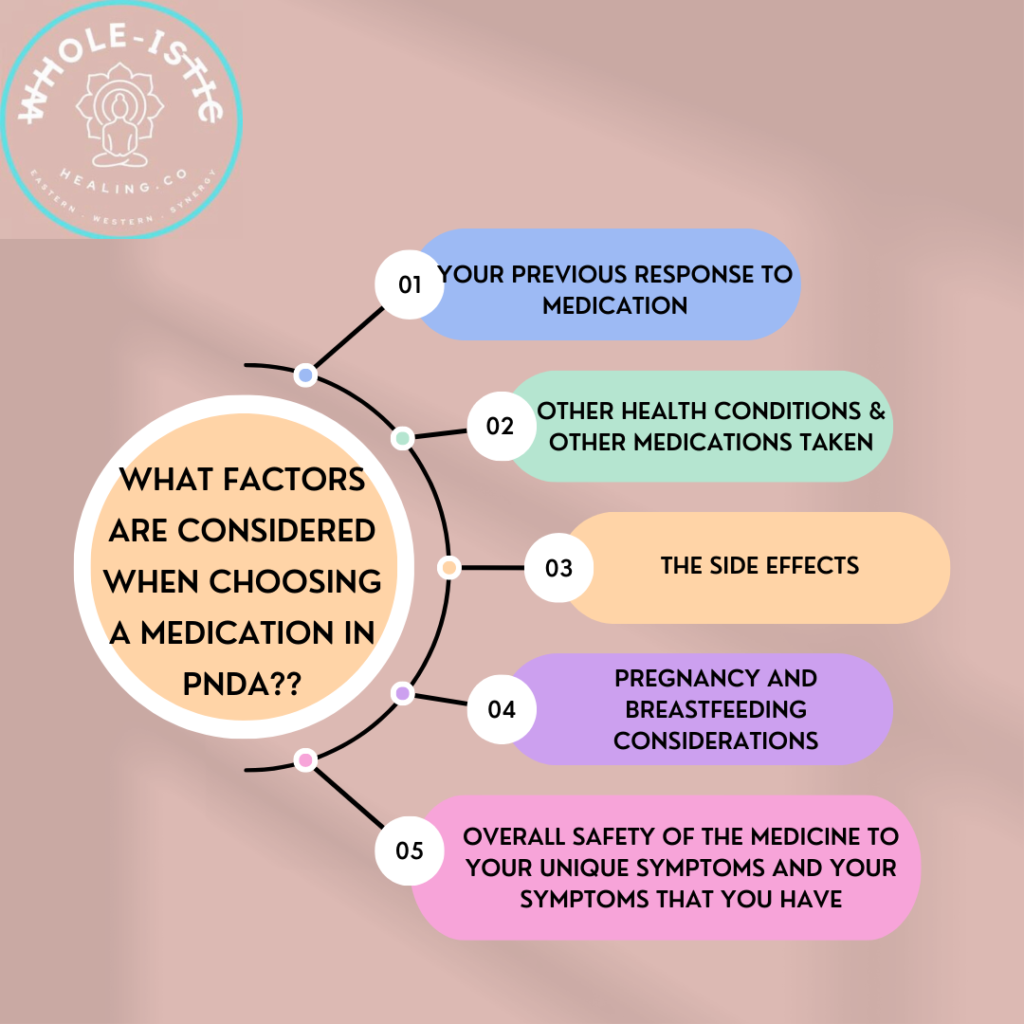
What factors are considered when choosing a medication?
Whilst your doctor will look at so much more, as a rough guide they would look into;
- your previous response to medication if you have used it before
- other health conditions, which may impact the safety of medications
- the adverse effects of the medication
- the potential for drug interactions
- the toxicity in overdose, and therefore the safety profile of the medicine and your unique presentation
You can see why it’s not a ONE SIZE fits all approach, and because a ‘friend’ had success with one class of medicine does not mean that it is right for you.
It is also important to know, that using one medicine successfully in the past does not guarantee effectiveness the second time; as was my case.
Not to be disheartened, but the extent of biochemical change can differ and potentially be more heightened with subsequent episodes or relapses. It may require higher doses, or additional agents or completely different class of medication to have the same effect…so to keep this in mind also.
According to the AMH (Australian Medicines Handbook), approximately HALF of adults (not specifically the postnatal cohort, but rather the general cohort), with moderate-to-severe major depression, respond to antidepressant treatment.
- Most antidepressants are approximately equal in efficacy; however individual responses vary significantly
- Can be a matter of TRIAL and ERROR to find your right medicine…patience will be a virtue here to go through the process
- What are some MYTHS around medications?
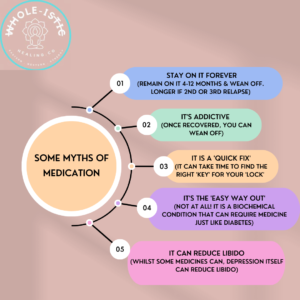
+ That it is addictive (it corrects underlying biochemistry & can be used in conjunction with psychotherapy. Once not required, it can be successfully weaned)
+ Once you start medication you are on it for life (as above)
+ It will make you a zombie with no heart or emotions/numb (for me, my biochemistry caused me to feel like a zombie and unable to make any decisions! Only once my biochemistry was repaired did I return back to my full vibrant self)
+ It can cause weight gain (some medicines can yes, however in some, depression can cause increased appetite and weight gain also)
+ Loss of libido (whilst this can be true for some medicines and some people’s response to medication, depression itself can also reduce libido)
+ People that live in a ‘low-tox’ manner, it feels like they are taking chemicals or foreign substances (the debunk to this is that medications can save lives, and certainly saved mine. I would rather be alive than to not be here, so it is a matter of balancing the risk vs benefit)
+Fear of being labeled as being on medication, the ‘fear’ of losing their registration if a health professional or being ‘found out’ (this is fear, to which the opposite of fear is unconditional love! Removing the fear of what ‘outside’ people or authorities might do or say; is to fill your hearts with compassion and love of what might be instead)
+ That it is a ‘quick fix’; (it may not be based on the indicated time frames it can take!)
+ That it is the ‘easy way out’ (not at all! Just like diabetes, medication corrects underlying biochemistry and there is no easy way out of that!)
+ Once healed that you won’t ever feel yourself without medication (not true at all! Once you have recovered, you only need to remain on it for 4-12 months and longer if you have relapsed; other than that, you are not bound to lifelong treatment!)
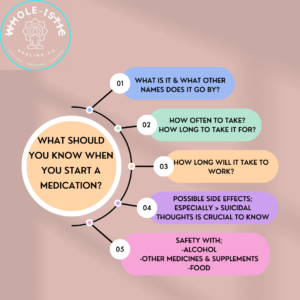
What should you watch out for or consider when beginning a new medication?
It is important before starting to know;
- WHAT it is? What other names does it go by? (so you don’t double up)
- HOW does it work?
- What are the side effects?
A NUMBER OF MEDICATIONS HAVE AN INCREASED SUICIDE RISK, SO THIS IS CRUCIAL TO KNOW UPON STARTING FOR YOU AND YOUR FAMILY/LOVED ONES. I go into this more in part 2, but knowing this allows your loved ones to be EXTRA vigilant; it can save lives knowing this…and having the health literacy around it (what to watch for, what to do, where to go)
- How long until it starts to work? How long to remain on the medication?
- What can it interact with; medicines and food?
- Can you drink alcohol with it?
- Any other questions you have
What are REALISTIC time frames of medications working?
Important to know that medications are not always a QUICK FIX; it can take time to work;
+ Begin with a low dose, and increase slowly if necessary over 2-4 weeks as tolerated
+ Some improvements within 1-3 weeks
+ Most improvement within 4-6 weeks
+ Full effects may take 6-8 weeks
Knowing this, provides REALISTIC expectations, which are SO important!
If after a time period, if your doctor deems that the medication is not working they may decide to;
- Increase the dosage
- Add another agent
- Wean off this medication slowly, and introduce a new medication altogether
It is VITAL however, to never decide yourself that it isn’t working and stop suddenly. This can cause severe side effects and it is needs to be ONLY done with close monitoring from your doctor based on WHAT they decide is best for you.
If it is not working, then open communication about WHAT your symptoms are and how you are feeling, will allow them to decide WHAT to do next. COLLABORATION is needed

HOW LONG DO YOU NEED TO REMAIN ON MEDICATION FOR?
The myth of needing to remain on medication for life, is a myth!
Generally speaking, once your symptoms have resolved on medication, you may need to remain on it for 4-12 months, depending on your physician. The time increases based on the number of relapses.
Again, NEVER cease medication without advice from your doctor…no matter how great you feel!
What should you consider in regards to the safe use of medicines?
+ Following from above, it is important to ALWAYS continue your medicines and never START/STOP at a whim, or because you feel better. You feel better because the medicines are recalibrating your biochemistry!
+ On this note, always ensure that you get your supplies in advance, so there is no risk of running out. Especially with various out-of-stock issues after the pandemic, it is important to ensure you have enough medicine to continue with.
In a situation where it is out-of-stock, ring around various pharmacies to locate stock and then have your script filled.
+ In terms of storage, especially with small children, it is VITAL to keep the medicines stored in a cool place ABOVE the REACH of CHILDREN and MINDFULLY focus whilst taking the medicine. It can be easily dropped & think crawling babies (ah!)…so concentrate so you know you have taken it and there is no risk of forgetting that you took it.
(Tick your calendar if you like that, or set a reminder on your phone that action immediately)
+ Always ensure when travelling that you take your medicines with you! I always take mine on hand-luggage too, so that there is no chance your bag will be lost and your pills too!
+ Do not keep them in a hot car; below 25 degrees Celsius and out of direct sunlight
What if the medication does not work for you?
+ Chat with your doctor FIRST
+ NEVER increase the dosage or cease medication on your own
+ Know that there are SO many options to try! Never feel despondent that nothing will work; you WILL find your KEY!
+ Be patient and hold onto faith that the right medication will be found
+ Make sure you listen to part 3 where I go through ‘whole-istic’ strategies to utilize whilst using Western treatments, to adjunct or compliment your treatment
+ Open communication with your doctor is key
+ Chat with your partner/loved one, and ask them how you have been tracking. You may not see any improvements, but they may! Open communication is key
+ Check in with yourself to try jot down specifically what/why you feel it is not working (sleep, appetite, mood, side effects etc.). This will help your health team decide WHAT is best for you
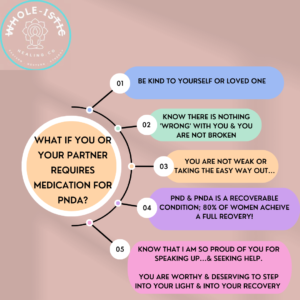
What if I need medication or your partner needs medication?
Firstly, be KIND to yourself or your partner.
Know, there is NOTHING wrong with you for needing medication.
You are NOT weak.
You are NOT taking the easy way out.
You are bold and taking action into your recovery.
Know that I am proud of you for trusting in your health professional, and that this piece may be the one that will save your life.
I would dedicate time to speak with your doctor about ANY and ALL questions that you have; as well as your pharmacist to go through ALL the information that you need!
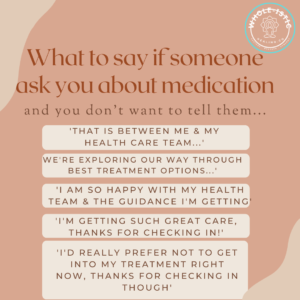
What can you say if your family or friends ask if you are on medication?
We all have the right to privacy and confidentiality; so we do not need to disclose any information to anyone that we don’t want to. Simple.
The disclaimer to this though for me personally is, is telling your loved ones that live with you if you begin medication so that they can monitor for any increased or changes to suicidal thoughts.
However, other than that, it is no one’s business if you don’t want it to be!
Examples of things to say if you don’t want to answer;
– ‘That is between me and my health care team’
– ‘We’re exploring our way through the best treatments, and I am happy with the care that I am receiving’
– ‘I am under excellent care with my health team, thank you so much for checking in’
If you do want to share with them that you are, then also, that is your choice and right to share what you want to!
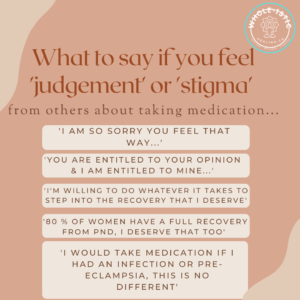
What to say if you feel judgement or stigma from others for taking medication?
I would tell them to F off! It is NO body else’s right to tell you what to do or to impose their feelings onto you and your health.
I would simply stand tall in your informed decision that you have made, with the conviction that you are taking action to walk towards your recovery and put it on them;
– ‘I am so sorry you feel that way…’
– ‘You are entitled to your opinion, but this is my body and my health, and I have the right to choose’
At the end of the day, no one else’s opinions matter except for those that are helping you through your recovery, the one’s holding your hand when you fall. The one’s who lay awake with you, or help carry the load when you cannot. Those are the only people that matter, not anyone else.
And if it is the same people who are judging you or imposing their man-made judgement around medication, then I would simply say that you are doing whatever it takes to recover from this condition, I am worthy and deserving to be back into my light…my children deserve that too.’
Simple.
80% of women fully recover from this, and I believe that with greater health literacy of what it is, what treatments are available and having the tribal support, that it can be 100%.
Do not let anyone’s ignorance keep you in the dark for any longer than necessary.
You are a being of light, and you are so deserving to walk back into your light.
Your life will feel brighter, more fulfilling and connected that before…I promise you.
You just have to keep on going and showing up.